I CAN: Integrate shift coaching into routine work at my center.
This program works best when launched using the same quality improvement strategies that your center employs to pilot test and scale new changes to clinical practice. This includes having a project team and using a data-driven approach to monitoring implementation.
Ideally, it doesn’t have a finite beginning and end, but reflects a new culture of mutual accountability where it’s valued when peers help each other to excel with infection control practices.
Implementing the program involves:
Create a team that is led by the infection preventionist and includes:
- Administrator
- Director of Nursing
- Director of Quality
- Secret Shopper
- One or more coaches
- Others, as needed
Identify someone responsible for scheduling meetings, recording decisions, and following up on them. Set the expectation that the work will be shared and that the team’s goal is to ensure that coaching becomes embedded in routine care delivery.
This team should follow the quality improvement model that your center uses to pilot test and scale new changes to clinical practice.
Including key decision makers or leaders is important, so that information about the program can be communicated broadly throughout your center and so that they can help to troubleshoot and remove barriers that arise.
Identify coaches, trying to ensure that you will always have at least one coach per shift and unit. The number of coaches that you need will depend on the size of your facility, schedules, and weekend coverage, but the goal is to prevent gaps in coaches across shifts and days.
Look for staff who:
- Are informal unit-based leaders, often helping others
- At times, serve as influencers
- Demonstrate excellence and commitment to infection control practices
- Support their coworkers’ education and training
- Will feel comfortable speaking up
Gold standard: Consider choosing certified nursing assistants: designating CNAs to be champions can increase participation in QI programs and improve job satisfaction, among other outcomes. Choosing managers, on the other hand, can make the interactions feel punitive — that’s not the intent and why we don’t recommend managers be coaches.
Other options: If you have CNA career ladders, you can incorporate the coaching role formally into growth opportunities. If you’re worried that designating some CNAs as coaches will leave others out, rotate the role so everyone has a chance to be a coach.
Whatever you do: ask coaches to participate; allow them to say no. You want people who will champion the work.
Using a coach roster can help with scheduling across shifts. Consider also posting or otherwise sharing the roster, so that coaches are recognized, aware who else is a coach, and can be resources for one another and their coworkers.
Ask coaches to review the coach guidance, and then conduct a brief follow-up training — or multiple sessions, across shifts — to discuss the guidance and what they will do, including what to look for on their shifts, how to offer feedback (whether corrections or praise), and how to share observations with you. Check their coaching knowledge, skills, and attitudes.
While this program doesn’t include infection control training, you may want to include an in-service to understand coaches’ baseline knowledge of infection control practices and to refresh their memories, particularly regarding any known infection control issues in your center. You may find this handout on knowledge, attitudes, and skills helpful.
Identify someone to audit adherence to infection control best practices. Look for a staff member who:
- Can easily be on any unit or neighborhood
- Has good observation skills
- Is comfortable working with numbers
As with the coaches, ask the secret shopper to participate; allow them to say no. You want people who will champion the work.
Ask the secret shopper to review the guidance for their role.
Invite them to be part of the team, so that they can participate in using the audit results to inform changes to the program and understand the vitally-important role that collecting these data plays in forming the feedback loop.
As you begin piloting and expanding the program, ask the secret shopper for their input:
- How long are the audits taking?
- What is the “right” frequency for conducting audits?
- How should the data be shared with your center’s QAPI program and leadership?
- Should there be more than one secret shopper to share the responsibility and time commitment?
Note that while the secret shopper may calculate adherence for you, they can also simply provide with the completed paper tools. This may be easier for them to do with their other responsibilities.
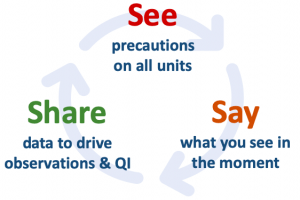
The I CAN feedback loop ("share") includes two types of data: (1) feedback from coaches about what they've observed and (2) the audit data captured by the secret shoppers. Both inform your guidance to the coaches about what to look for ("see") on the units.
The infection preventionist is the point-person for the communication with coaches and should determine the best strategy. We recommend that they conduct quick huddles, or stand-up meetings, with the coaches each day to learn from them and direct their focus. Huddling is an evidence-based practice to improve communication.
If huddling isn't possible, the infection preventionist guidance provides other options.
The project team should share information and results from the program with your COVID-19 team, administrator, and others in leadership who can reinforce infection control practices, allocate resources where needed, and otherwise champion the program to ensure its success.
Don’t forget: We need your help! I CAN is free, but we ask you to share your contact info when you begin so that we can follow-up with a brief assessment after several months.we need your help!