We are interested in understanding how one lung disease affects the response to a secondary insult in ether the lung or in a distal part of the body. Using clinically relevant model systems we examine the impact of the lung microbiome on pulmonary diseases, alterations of the immune response during pulmonary viral/bacterial coinfection, and the lung epithelial/endothelial responses during lung infection, damage, and disease. The overall goal of our research is to understand how the lung influences systemic responses.
1) Host resilience to lung infection and injury:
Pneumonia is the leading cause of death from infection of children under five. It is higher than deaths caused by HIV, Malaria, or even diarrheal diseases (UNICEF/WHO, 2006, Pneumonia: The Forgotten Killer of Children). In addition, recent pandemics have shown us that lung infections spread easily and cause significant morbidity and mortality. Influenza virus is a leading cause of viral pneumonia, and a common clinically relevant complication of influenza virus infection is bacterial pneumonia. In addition to influenza A virus/bacterial coinfections we are studying how SARS-CoV-2 infection in the lung causes systemic changes including coagulation. We are studying the impact of e-cigarette aerosols on both the pulmonary immune response and the resilience response. We have developed in vivo and in vitro models to study complex respiratory infections, and we are also analyzing patient samples.
2) Airway microbiome
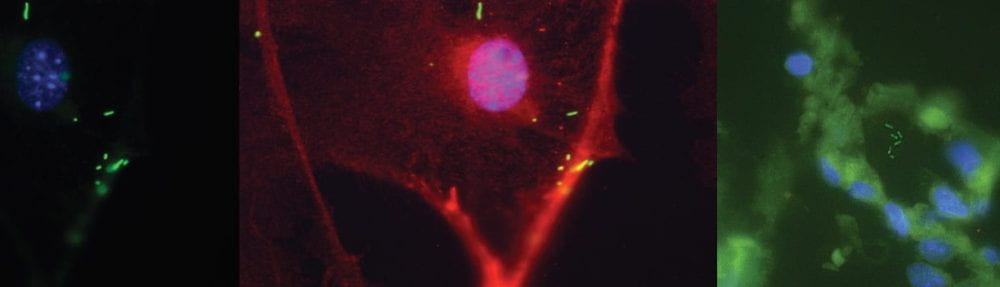
Another research interest of the lab is to understand changes that occur in the airway microbiome during lung diseases. The field of the airway microbiome is an emerging field, and as such we have had to develop several new techniques, and adapt techniques used for other microbiomes to this unique space. We are interested in the microbiome of the lung tissue. We aim to the composition of the airway during health and disease, including cancer and infection, and how changes in composition impact the overall health of the host.
3) Immune Triage: Understanding Host resilience to Infection and Trauma
The development of pneumonia in trauma and post-surgical patients leads to increased morbidity and mortality. Lung infections occur for diverse reasons in a hospital setting, but the impact that pneumonia onset has on wound healing responses has not been examined. This project seeks to examine the concept of immune triage, in that when faced with a healing wound and an infection at disparate sites the host must be able to deal effectively with both insults, and at times prioritize responses. We are using several cutaneous and subcutaneous trauma models that allow us to look at the wound healing response, vascularization, and neural interactions.