What is Pulse Oximetry?
- Pulse oximetry is a painless, non-invasive technique used globally to estimate oxygen saturation (Sao2) within the bloodstream

- Oxygen saturation values of 95% to 100% are generally considered normal. Values under 90% could quickly lead to a serious deterioration in status, and values under 70% are life-threatening
- Pulse oximetry is regularly used across a broad range of health care settings to determine how well your lungs are transporting O2 to your body (i.e. used to continuously measure the 4th vital sign)
How do Pulse Oximeters work?
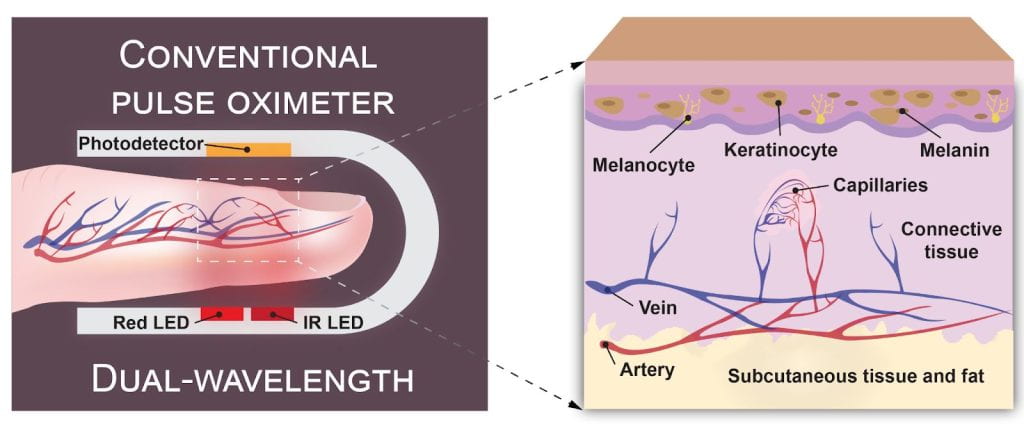
- Pulse oximeter (pulse ox) sensors consist of two or more wavelengths, photodetector(s) and an algorithm that leverages empirically-derived values to estimate peripheral oxygen saturation (SpO2)
- The light-based technique measures changes in light absorption due to blood volumetric variations during the cardiac cycle, which is commonly referred to as photoplethysmography (PPG)
- The sensor probes clip onto a translucent body part and are configured to operate in transmission (e.g. through the finger or earlobe) or reflection (e.g. at the wrist) mode and provides a percentage amount of oxygen in the blood
- Relative changes in light absorption between oxygenated and deoxygenated hemoglobin chromophores can be evaluated by a ratiometric comparison between the wavelength dependent time-varying PPG signals after interacting with living tissue that is dominated by light scattering
Issues with Pulse Oximeters
- Pulse oximetry is less precise than conventional direct methods, such as ABG testing
- Pulse ox’s are precisely calibrated between 70 – 100% using controlled desaturation studies however the presence of many other chromophores can impact the PPG signal quality and SpO2 accuracy: e.g. carboxyhemoglobin (COHb), methaemoglobin (MetHb), keratinocytes and melanin
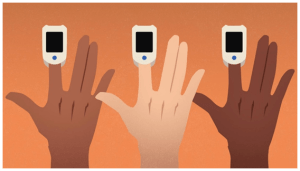
- Biases in oxygen saturation measured by pulse oximetry (Spo2), when compared with arterial oxygen saturation (Sao2) measured by arterial blood gas (ABG), have been observed in many retrospective and retrospective studies depending on the amount of melanin present in the epidermal layer of the skin
History
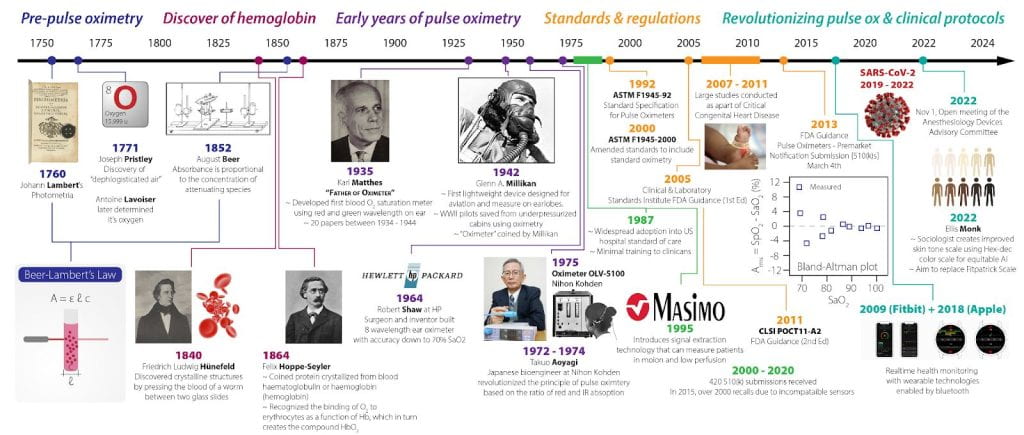
- It marks half a century since Takuo Aoyagi revolutionized the principle of pulse oximetry based on the ratio-of-ratio method used red and infrared light
- The FDA held an advisory committee meeting of the Anesthesiology and Respiratory Therapy Devices Panel of the Medical Devices Advisory Committee to address the recent reports of racial bias in pulse oximeters during COVID-19
Our Approach
- We aim to address the deleterious effects of skin pigmentation on pulse pulse oximeters by leveraging advanced polarization and wavefront engineering techniques
PREVIOUS PUBLICATIONS
Single-wavelength, single-shot pulse oximetry using an LED-generated vector beam

Conventional pulse oximetry estimates the ratio of light absorbed at two wavelengths. Attempts have been made to improve the precision of these measurements by using polarized light, with the tradeoff of requiring multiple sequential measurements. We demonstrate a novel pulse oximetry technique that uses radially polarized light generated by a light-emitting diode (LED) to obtain single-shot, blood oxygen-saturation measurements using a single wavelength at a rate of 50 fps. Our work, to the best of our knowledge, presents both a novel use of a vector beam and a first demonstration of vector-beam generation using LEDs measured on 5 healthy young adults.
Opt. Express 30, 27293-27303 (2022)
Our research team is dedicated to exploring new frontiers in pulse oximetry technology and its applications in improving patient outcomes. By collaborating with us, you can contribute your skills and resources to drive meaningful advancements in healthcare.
Interested in learning more? Reach out to us at pulseoxstudy@brown.edu to explore collaboration opportunities. Together, let’s make a difference in healthcare!