Author: Daniel Chan
ABSTRACT: THE GROWING BURDEN OF CHRONIC KIDNEY DISEASE
As the ninth leading cause of death in the United States,1 kidney disease undoubtedly deserves our increased attention through novel research. According to the Centers for Disease Control and Prevention, 37 million (or 1 in 7) American adults live with chronic kidney disease (CKD)1. In fact, more than 90% of adults with CKD are unaware of its presence and harmful health effects1. Therefore, CKD’s status as a “silent killer” exacerbates its high prevalence, evades its medical surveillance, and leads to poor health outcomes in those living with kidney disease in the United States.1,2
One of the primary predictors of CKD health outcomes is the accessibility and early implementation of preventive care measures.3,5,6 In particular, kidney disease screenings hold great promise in the early detection of CKD for three reasons:5,6 1) CKD is amenable to screening, as it has a long asymptomatic phase (on the scale of years), 2) only 10% of individuals with CKD are aware of their diagnosis, and early interventions have been proven to reduce the risk of CKD progression, and 3) CKD screening tools–such as urine albumin or serum creatinine tests– are fast, convenient, and can be readily integrated into patient care.
Such preventive disease screening is understudied and not yet established as a routine part of patient care in the United States. For example, the U.S. Preventive Services Task Force provides “no recommendation” to screen for CKD in asymptomatic adults due to inadequate evidence of tangible benefits and improved clinical outcomes.7 In comparison, other nations, such as Taiwan, have taken the initiative to establish extensive CKD surveillance programs that have resulted in early disease detection and improved health outcomes for CKD patients.3
Here, we compare and contrast the nature of the healthcare systems of the United States and Taiwan, which both report some of the highest rates of kidney disease in the world. Both countries bear similar levels of CKD morbidity, but demonstrate opposing trends in CKD mortality. Although both countries experience a high burden of CKD, Taiwan has maintained a steady decrease in deaths due to CKD, while the United States has reported a sharp increase in CKD mortality over the past 30 years.10 The renal care delivery, health system structures, and healthcare policies vary greatly between the two nations, which may explain their observed differences in CKD care accessibility, preventive care implementation, and patient outcomes. This paper aims to compare and contrast kidney disease care strategies between the US and Taiwan, examine their resulting effects on CKD epidemiology, and identify the defining characteristics of a successful CKD care system that can be incorporated into future CKD care practices.
BACKGROUND: THE LANDSCAPE OF CKD CARE IN THE UNITED STATES
The early detection of CKD holds major public health implications within the US. According to the Centers for Disease Control and Prevention, 37 million (or 1 in 7) American adults currently live with chronic kidney disease.1 In fact, more than 90% of adults with CKD are unaware of its presence and harmful health effects.1 Therefore, CKD’s status as a “silent killer” fuels its high prevalence, evades its medical surveillance, and leads to poor health outcomes in those living with kidney disease.1,2 In addition, CKD represents a significant economic burden in the US, where non-dialysis CKD patients account for nearly 20% of all Medicare spending,24 more than $81 billion is spent per year treating kidney disease in Medicare beneficiaries,26 and CKD incurs a cost of approximately $22,348 per person per year in medical expenditures.24
Among Americans, the distribution of CKD also falls along racial and socioeconomic lines: for example, African-Americans suffer from kidney failure at 3 times the rate of White Americans.4 These disparities are exacerbated by the high prevalence of other chronic disease comorbidities in the general population, such as obesity, diabetes, and cardiovascular disease— all of which contribute to the rising incidence of CKD in the United States.1,2 The disease trajectories of CKD patients in the US are further worsened by the sporadic accessibility of preventive care and the difficulty associated with navigating the complex American healthcare system.6,8,9 Within the US, primary care physicians play a “gatekeeper” role in controlling a patient’s access to specialist care, which can discourage individuals from engaging with renal care services.6,8,9 In addition, the multi-payer reimbursement structure of the US healthcare system leads to inconsistent health coverage between different patients.8 Together, the gatekeeper function of primary care providers and the variable coverage of private insurance interact synergistically to disincentivize individuals with CKD from seeking renal care and disease screening services from nephrologists.5,6,7
Furthermore, previous studies of various healthcare industry stakeholders have found that the conflict between financial incentives and chronic disease prevention has led to an “implementation gap” of preventive healthcare services in the United States, where the prospect of financial gain discourages hospital systems from practicing preventive medicine such as disease screening and patient education.8 Therefore, unlike other chronic diseases such as cancer, kidney disease screening is not widely practiced in the US, which may contribute to the common late-stage detection and poor health outcomes of CKD patients.5,6 For example, current CKD care protocols do not direct physicians to utilize preventive care measures. In particular, the U.S. Preventive Services Task Force provides “no recommendation” to screen for CKD in asymptomatic adults due to inadequate evidence of tangible benefits and improved clinical outcomes.7 Patients also report significant barriers to healthcare access in the US, such as high costs and inadequate insurance coverage, which are characteristic of the complicated, multi-payer American healthcare system.8 Therefore, such structural barriers in healthcare access pose additional threats to the provision of preventive healthcare services for CKD patients in the United States.
TAIWAN: A CASE STUDY OF SUCCESS IN CKD CARE AND PREVENTION
On the other side of the Pacific, Taiwan (the Republic of China, R.O.C.) experiences similar challenges with CKD: the island nation exhibits the world’s highest prevalence and incidence rates of end-stage renal disease (ESRD)— a latter phase of CKD wherein kidney failure requiring dialysis occurs.10,11,12 In Taiwan, an estimated 2.5 million people live with CKD, and 3392 individuals per 1 million in the general population experience kidney failure (Table 1)—a prevalence of ESRD more than 1.5 times that of the United States.18 However, compared to the US, Taiwan has taken proactive steps to stem the growth of kidney disease.
In particular, the nature of the Taiwanese healthcare system has allowed it to smoothly and successfully implement CKD prevention and mitigation measures. Firstly, as a nation with a single-payer healthcare system, Taiwan provides medical care with high accessibility, efficiency, affordability, and value.13,14 In a system characterized by good accessibility, comprehensive coverage, short waiting times, and low costs, Taiwan’s national health insurance program and care services can be best described as “cheap and abundant.”14
In this healthcare environment, the government has established initiatives such as the Family Practice Integrated Care Project (FPICP)13,14 to integrate primary patient care with preventive and specialty services. Within these programs, community networks enable disease management, health education, specialist care, and preventive care to be integrated into a patient’s primary care routine. This mode of integrated healthcare delivery ensures that people can receive a full continuum of “health promotion, disease prevention, diagnosis, treatment, and disease management.”15,16 As a result, individuals are empowered to take charge of their personal health and actively engage with care providers, rather than being passive recipients of services. These preventive care measures enable clinicians to detect kidney disease in its early stages and educate patients so that CKD progression is slowed or even stopped.3 In this way, patients are driven to be active seekers of preventive CKD care,16,17,18 which is correlated with improved disease trajectories and reduced mortality and overall disease burden due to CKD.3, 21
Given the high rates of CKD/ESRD in Taiwan, the field of kidney medicine has served as a natural launching pad for these integrated healthcare services. In 2001, the Taiwan Society of Nephrology partnered with the Taiwanese Department of Health to launch the multidisciplinary predialysis education (MPE) initiative, which promotes the screening of high-risk populations for CKD, health literacy education, multidisciplinary team care, and integration of renal care into other medical specialties.18 With the backing of a single-payer national healthcare system, as well as a culture of integrated care, the MPE initiative has demonstrated sustained success in decreasing CKD patient mortality, ESRD incidence, as well as total medical expenditures (due to decreased utilization of inpatient renal care) throughout Taiwan.3,18,21
Despite the high prevalence and incidence of kidney disease in Taiwan, the country has also managed to provide quality and cost-effective care to CKD patients. Taiwan spent an estimated $1.8 billion25 on CKD-related care in 2019 on an estimated CKD patient population of 2.5 million individuals21— representing a much smaller per-person cost in CKD-related medical spending compared to the United States’ $22,348 per person per year.24 Public health officials and physicians attribute these lowered costs to Taiwan’s investments in early-detection systems for CKD and the incorporation of renal care into general medical practice.3,21
COMPARING TRENDS IN CKD PREVALENCE, INCIDENCE, AND MORTALITY BETWEEN THE UNITED STATES AND TAIWAN
Upon examination of the cross-national differences in CKD prevention, treatment, and patient outcomes between Taiwan and the US, many of these disparities find their roots in the functional differences between the two countries’ healthcare systems. Particularly, the comprehensive, integrative, and plentiful nature of Taiwanese healthcare means that in comparison to the US, the early detection and prevention of CKD are more common and easily achieved in Taiwan. International epidemiological data for CKD/ESRD from the last 30 years reflects consistent improvements in CKD mortality in Taiwan, while the US has reported significant increases in mortality due to kidney failure (Table 1),11,12,19 which is consistent with the widespread use of CKD prevention measures in Taiwan and its comparative absence in the United States.
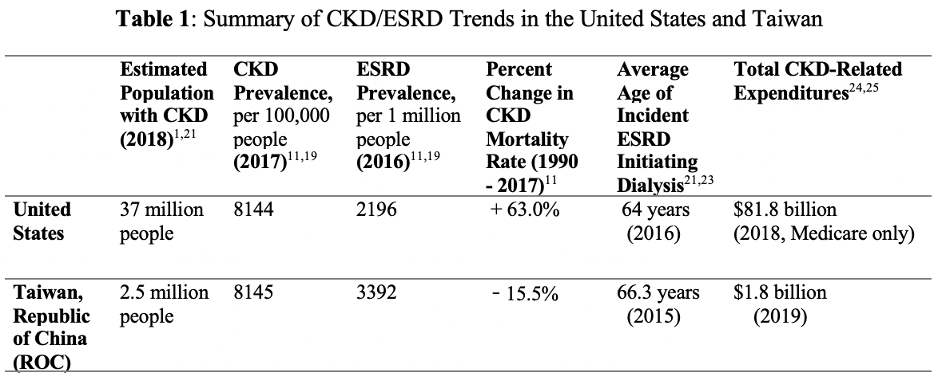
In 2017, Taiwan reported a CKD prevalence of 8145/100,000 people (in the general population),11 and the US reported a similar rate, with 8144/100,000 individuals in the US suffering from CKD (Table 1).19 Despite these comparable values of CKD prevalence, the proportion of their respective populations that suffer from advanced kidney disease (i.e., ESRD) differ significantly. In 2016, Taiwan reported the world’s highest treated ESRD prevalence of 3392 per million in the general population (PMP),11 while the US saw an ESRD prevalence value of 2196 PMP (Table 1).19 Additionally, between 2003-2016, Taiwan’s treated ESRD prevalence rose by 122 persons PMP per year— the fastest rate of any country in the world.11 Upon initial analysis, Taiwan demonstrates seemingly poorer disease trajectories for CKD patients than the US, with a much greater proportion of individuals developing kidney failure through ESRD. However, although the rate of kidney failure is much higher in Taiwan than the US, their trends in mortality due to kidney disease are moving in opposite directions: the CKD mortality rate has decreased in Taiwan by 15.5% between 1990 and 2017, while it has increased by 63.0% in the US during the same period (Table 1).11
These trends provoke us to think about CKD development in terms of an illness-death model, which is a common multistate framework used in chronic disease epidemiology to describe disease progression and to study relations between the prevalence and incidence of a health condition.22 In the illness-death model of CKD, the clinical progression of kidney disease can be thought of as a triangle, where the patient’s chronic condition— kidney disease— is located at one vertex, and its two possible outcomes— either death or ESRD (i.e., kidney failure)— lie at the other two vertices (Figure 1).
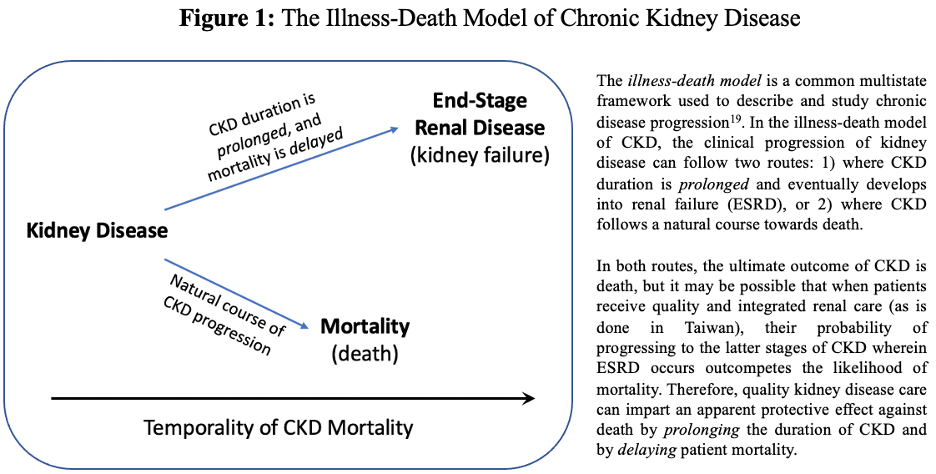
When kidney disease patients receive high-quality renal care, their probability of progressing to the latter stages of CKD wherein ESRD occurs outcompetes their likelihood of death. The ultimate outcome of CKD is death, but the provision of effective renal care (i.e., early CKD detection via disease screening, targeting of high-risk individuals, etc.) can impart an apparent protective effect against mortality by prolonging the duration of CKD (such that it can advance towards ESRD) and by delaying the onset of mortality in CKD patients. Therefore, the high incidence of ESRD in Taiwan may actually result from the preventive, integrated, and quality care that kidney disease patients receive, as well as the early detection of CKD through community health programs like the multidisciplinary predialysis education initiative.10,18,22
This becomes evident when one compares the average age of incident ESRD initiating dialysis (i.e., the average age at which dialysis begins for CKD patients) between the US (64 years)23 and Taiwan (66.3 years)21 (Table 1). Although this difference of 2.3 years in the average age of dialysis onset may seem small, it represents significant potential saved medical costs and improved CKD care timelines and patient outcomes. In a hypothetical situation where the US implements preventive CKD care strategies like Taiwan, millions of Americans with CKD could have their kidney health closely monitored so that renal failure and the use of dialysis are delayed. Hemodialysis currently costs the Medicare system an average of $90,000 per patient annually in the United States for a total of $28 billion.27 Consequently, improved CKD maintenance and the delayed onset of ESRD could save the American medical system billions of dollars in spending.
CONCLUSIONS AND FUTURE DIRECTIONS: LESSONS LEARNED FROM TAIWAN AND LOOKING AHEAD TO RENAL CARE REFORM IN THE US
Although current literature on comparative health systems in the context of CKD is relatively limited, we can see the clear impact of health system structure and healthcare organization on the outcomes of kidney disease patients through our comparative analysis of CKD care priorities in Taiwan and the US. The systemic distinctions between Taiwan’s navigable single-payer healthcare system and the United States’ relatively disjointed multi-payer system can in part explain the observed differences in the epidemiology and prognosis of CKD/ESRD between the two countries. These underlying differences in health system organization, healthcare delivery, and health policies may help explain the two countries’ opposing trends in CKD mortality.
Specifically, Taiwan’s CKD prevention and treatment strategies may prolong the lifespan of CKD patients, making them more likely to reach the latter stages of CKD wherein kidney failure occurs, and thus artificially inflate the recorded rates of ESRD in Taiwan. This provides a critical opportunity to use a learning healthcare system approach, where new evidence, best practices, and knowledge generation are actively embedded into daily medical practice to produce continual improvement in patient care.21 Identifying the successes of Taiwan’s CKD care strategies will allow public health officials to develop systemic reforms that American healthcare practitioners can use to improve the quality and accessibility of renal care in the US.
There are three points of interest in the Taiwan-US healthcare interface that are worth further exploration and trans-national exchange: 1) the effect of Taiwan’s healthcare system organization on kidney disease prevention, treatment, and patient outcomes, 2) the differences in the culture and administration of clinical renal care between the US and Taiwan, and 3) making novel comparisons between the Taiwanese and American healthcare systems in terms of policy, structure, and health outcomes. In particular, different practices and societal factors between the two countries seem to be driving vastly different outcomes in CKD mortality and patient wellness. Through a continued comparative health systems approach, it may be possible to identify the successful aspects of Taiwan’s approach to CKD care and assess how they can inform the improvement of renal care systems in the US. Channeling these novel findings from Taiwan into a learning healthcare system can help inform scientific and medical communities in the US about the best policies and practices that can be used to minimize the occurrence of new cases of kidney disease, as well as maximize the quality of life for Americans living with CKD/ESRD.
In particular, it will be vital for the US to study and adopt preventive care measures from Taiwan, such as early disease detection and predialysis patient education. Taiwan’s heavy investment in the primary and secondary prevention of CKD contrasts sharply with the United State’s strategy of tertiary prevention for kidney disease. Current care practices in the US focus on treating CKD in its latter stages, while preventive measures are chronically understudied in and are not yet established as a routine part of CKD patient care. Few longitudinal investigations of early CKD detection have been performed in the US, which has discouraged the medical community from recommending routine disease screening. However, as our investigation of kidney disease in Taiwan suggests, CKD screening and preventive care programs have the potential to detect disease early and improve health outcomes for CKD patients.3,21 These conclusions warrant a reexamination of CKD screening practices in the United States in order to improve renal care, support clinical decision making, and advance patient health.
Subsequent cross-national studies of kidney disease should continue to examine the current state of renal care in the US in tandem with intuition drawn from reviewing Taiwanese CKD data. In particular, it will be vital to account for baseline differences in population demographics and socio-cultural factors that may have confounding effects on the observed differences in patient outcomes between the two countries. However, this preliminary review and analysis of the care practices, structural differences, and epidemiological patterns of CKD among the US and Taiwan point to a strong association between health system organization and health outcomes of CKD patients. These meaningful inferences regarding the impact of cross-national factors on the health outcomes of CKD/ESRD patients will hold great utility in enhancing the strength and future of kidney medicine in the United States.
REFERENCES
- “Chronic Kidney Disease in the United States, 2021”, Centers for Disease Control and Prevention (CDC) (2021), https://www.cdc.gov/kidneydisease/publications-resources/ckd-national-facts.html
- “Chronic Kidney Disease”, Office of Disease Prevention and Health Promotion, Healthy People 2020 (2020), https://www.healthypeople.gov/2020/topics-objectives/topic/chronic-kidney-disease
- Hwang, Shang-Jyh et al. “Epidemiology, impact and preventive care of chronic kidney disease in Taiwan. Nephrology.” 3rd Asian Forum of CKD Initiative, The Official Journal of the Asian Pacific Society of Nephrology (APSN) .15: 3-9 (2010). https://doi.org/10.1111/j.1440-1797.2010.01304.x
- “African Americans and Kidney Disease”, National Kidney Foundation (2016), https://www.kidney.org/news/newsroom/factsheets/African-Americans-and-CKD
- Saunders, Milda R et al. “Screening for Chronic Kidney Disease.” JAMA 314,6 (2015): 615-6. doi:10.1001/jama.2015.9425
- Berns, Jeffrey S. “Routine screening for CKD should be done in asymptomatic adults… selectively.” Clinical journal of the American Society of Nephrology : CJASN 9,11 (2014): 1988-92. doi:10.2215/CJN.02250314
- “Screening for Chronic Kidney Disease: Recommendation Statement”, S. Preventive Services Task Force (2014), https://www.aafp.org/afp/2014/0215/od1.html
- Levine, Susan et al. “Health Care Industry Insights: Why the Use of Preventive Services Is Still Low.” Preventing chronic disease 16 E30. 14 Mar. 2019, doi:10.5888/pcd16.180625
- Cueto-Manzano, Alfonso M et al. “Comparison of primary health-care models in the management of chronic kidney disease.” Kidney international supplements 3,2 (2013): 210-214. doi:10.1038/kisup.2013.16
- “Nationwide CKD Prevention Project and Outcome in Taiwan”, Taiwan Society of Nephrology (2010). https://archive.theisn.org/images/taskforce/Taiwan/Nationwide%20CKD%20Prevention%20Project%20and%20Outcome%20in%20Taiwan.pdf
- Yang, Chih-Wei et al. “Global case studies for chronic kidney disease/end-stage kidney disease care.” Kidney international supplements 10,1 (2020): e24-e48. doi:10.1016/j.kisu.2019.11.010
- Bikbov, Boris et al. “Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017.” The Lancet, Volume 395, Issue 10225, 709 – 733 (2020). https://doi.org/10.1016/S0140-6736(20)30045-3
- Donnelly, Peter D et al. “Single-Payer, Multiple-Payer, and State-Based Financing of Health Care: Introduction to the Special Section.” American journal of public health 109,11 (2019): 1482-1483. doi:10.2105/AJPH.2019.305353
- Wu, Tai-Yin et al. “An overview of the healthcare system in Taiwan.” London journal of primary care 3,2 (2010): 115-9. doi:10.1080/17571472.2010.11493315
- Jan, Chyi-Feng et al. “A 10-year review of health care reform on Family Practice Integrated Care Project-Taiwan experience.” Family practice 35,4 (2018): 352-357. doi:10.1093/fampra/cmx111
- Li-Lin Liang, Impact of integrated healthcare: Taiwan’s Family Doctor Plan, Health Policy and Planning, Volume 34, Issue Supplement_2, November 2019, Pages ii56–ii66, https://doi.org/10.1093/heapol/czz111
- “What are integrated people-centred health services?”, World Health Organization (WHO) (2020), https://www.who.int/servicedeliverysafety/areas/people-centred-care/ipchs-what/en/
- Yu, Yu-Jen et al. “Multidisciplinary predialysis education reduced the inpatient and total medical costs of the first 6 months of dialysis in incident hemodialysis patients.” PloS one 9,11 e112820. 14 Nov. 2014, doi:10.1371/journal.pone.0112820
- “Chapter 11: International Comparisons, 2018 USRDS Annual Data Report”, United States Renal Data System (USRDS)(2018), https://www.usrds.org/media/1738/v2_c11_intcomp_18_usrds.pdf
- “Chapter 3: Morbidity and Mortality in Patients with CKD, 2016 USRDS Annual Data Report”, United States Renal Data System (USRDS) (2016), https://www.ajkd.org/article/S0272-6386(17)30077-X/pdf
- Wu, Mei-Yi, and Mai-Szu Wu. “Taiwan renal care system: A learning health-care system.” Nephrology (Carlton, Vic.) 23 Suppl 4 (2018): 112-115. doi:10.1111/nep.13460
- Vejakama, P., Ingsathit, A., McEvoy, M., Attia, J., & Thakkinstian, A. (2017). Progression of chronic kidney disease: an illness-death model approach. BMC nephrology, 18(1), 205. https://doi.org/10.1186/s12882-017-0604-8
- “What are the pros and cons of undergoing kidney dialysis? If you are not a candidate for a kidney transplant, how long can you remain on dialysis?”, American Association of Kidney Patients (AAKP) (2010), https://aakp.org/what-are-the-pros-and-cons-of-undergoing-kidney-dialysis-if-you-are-not-a-candidate-for-a-kidney-transplant-how-long-can-you-remain-on-dialysis/
- Ozieh, M. N., Bishu, K. G., Dismuke, C. E., & Egede, L. E. (2017). Trends in healthcare expenditure in United States adults with chronic kidney disease: 2002-2011. BMC health services research, 17(1), 368. https://doi.org/10.1186/s12913-017-2303-3
- “Chronic kidney disease costs nation NT$53.3bn”, Taipei Times (2020), https://www.taipeitimes.com/News/taiwan/archives/2020/07/13/2003739828
- “Chronic Kidney Disease Basics”, Centers for Disease Control and Prevention (CDC) Chronic Kidney Disease Initiative (2021), https://www.cdc.gov/kidneydisease/basics.html
- “The Kidney Project, Statistics”, University of California San Francisco (UCSF) (2018), https://pharm.ucsf.edu/kidney/need/statistics