By Samiyra F. Afife
Introduction
Non-communicable Diseases – Looking at Cardiovascular Disease in Morocco
In global public health, the rise of non-communicable diseases (NCDs) has become a difficult challenge—fundamentally altering the narrative of healthcare worldwide. These conditions, encompassing a diverse spectrum, including cardiovascular diseases (CVDs), cancer, chronic respiratory ailments, and diabetes, now constitute a staggering 70 percent of all deaths globally – a concerning statistic.¹
One region facing its battle with the NCD epidemic is Morocco, where the impact of these diseases on cardiovascular health is particularly pronounced. Cardiovascular NCDs, such as heart disease and stroke, are not only the leading causes of death globally but have also become a prevalent concern in Morocco. Cardiovascular diseases, comprising conditions like coronary heart disease and stroke, are strongly influenced by avoidable behaviors like poor dietary choices, physical inactivity, tobacco use, and excessive alcohol consumption. These behaviors can result in adverse health outcomes such as high blood pressure, elevated blood glucose levels, abnormal lipid levels, and weight-related problems.²
Cardiovascular health poses a significant challenge in many regions, with Morocco being no exception. The prevalence and awareness of hypertension and cardiovascular diseases, which affect even youth, remain pivotal issues.³ Notably, it was reported in the findings that these NCDs account for a staggering 38 percent of the overall 80 percent mortality rate in Morocco (Figure 4).⁴ The underdiagnosis of hypertension within sampled populations raises questions about the broader extent of undiagnosed cases within the country. These concerns underscore the necessity for public health initiatives aimed at raising awareness and understanding these non-communicable diseases.
NCDs significantly burden both the Arab region and Morocco’s healthcare system, adding to the issue’s complexity.⁵ The strain on healthcare resources and the financial implications are pressing matters that call for comprehensive strategies to address NCDs effectively. Despite remarkable progress in enhancing healthcare access for mothers and children in Morocco,⁶ challenges persist: notably socioeconomic disparities and health inequities. Recognizing these disparities is essential to ensure that improved healthcare access equitably benefits all Moroccan population segments.
Following the idea of socioeconomic disparities in Morocco’s regions, findings from research on Moroccan immigrants in the Netherlands present an intriguing finding that obesity is more common in Moroccan migrant groups in Europe than among the populations of the countries they have emigrated to.⁷ However, Moroccan immigrants exhibit lower rates of hypertension and cardiovascular diseases, which may be attributed to the accessibility and quality of the Dutch healthcare system compared to Morocco’s. These findings prompt a broader examination of healthcare accessibility and quality as a crucial factor in addressing cardiovascular diseases and health disparities.
Morocco, like many nations, aspires to achieve Sustainable Development Goal 3 – ensuring a healthy life and well-being for all.⁸ According to a Sustainable Development Report for Morocco, considerable challenges persist in achieving this goal, largely due to the widespread impact of cardiovascular NCDs. It was revealed that over 80 percent of deaths in Morocco are attributed to NCDs, with cardiovascular diseases at the forefront.⁹
The intricate interplay between the high prevalence of cardiovascular NCDs and the inadequacies within Morocco’s healthcare system becomes all too apparent. The nation finds itself at a critical juncture necessitating a comprehensive examination of its readiness to confront the cardiovascular NCD epidemic. Moreover, an essential aspect of this exploration will be the evaluation of healthcare inequities and accessibility, as these factors play a pivotal role in bridging the divide and reinforcing Morocco’s primary care framework.
This paper focuses on Morocco’s unique struggle with cardiovascular NCDs and their intricate interplay with the nation’s healthcare system. More specifically, this paper will examine the prevalence and impact of cardiovascular diseases in Morocco, the readiness and capacity of Morocco’s healthcare system, and the exploration of potential interventions and health inequities. Through this, there is an aim to better understand the dynamics of cardiovascular NCDs and contribute to the discourse on strengthening healthcare systems to address this alarming public health challenge in Morocco.
Methods
To conduct my literature search, I utilized Bruknow and the PubMed Database. In the search for viable resources and literature, the keywords: “Morocco”, “Cardiovascular Disease”, “Healthcare System”, “Healthcare”, “Education”, and “Non-communicable Diseases”, “NCD” were utilized. With searching “Morocco Cardiovascular Disease”, there were 624 results on the BruKnow database. Most of the peer-reviewed articles that arose from the results were viable resources that highlighted one or more of the following: prevalence and impact of cardiovascular diseases in Morocco, the readiness and capacity of Morocco’s healthcare system, and the exploration of potential interventions and health inequities. However, many of the non-peer-reviewed resources referred to inapplicable information (unrelated publications, scientific information regarding the human body, etc.) pertaining to my research question.
In conducting my literature search on the PubMed Database, the same keywords were utilized. With searching “(Morocco[Title]) AND (Cardiovascular Disease[Title/Abstract])”, there were 14 results on the PubMed database. Regarding literature selection, I excluded publications that focused on specific research questions and concerns regarding those specific questions. I selected publications that highlighted cardiovascular disease in Morocco, Morocco’s healthcare system, and initiatives to address health concerns (specifically cardiovascular disease and NCDs) in Morocco. Most of the selected articles and publications were published in the past thirteen years due to the lack of research initiatives regarding NCDs in Morocco. The findings from these sources were synthesized, critiqued, and analyzed to reflect and respond to my research question. The entirety of my methods and selection process is available in Figure 1.
Results
With the vast amount of varying information from the articles, navigation support is provided in Figure 2. This overview figure includes each reference utilized, a title, purpose, and methods for each reference. In this section, each reference will be developed in reference to the results and overall synthesis of each article. Across all articles, the trends are distinguished into three categories: the burden of cardiovascular NCDs in Morocco, challenges in Morocco’s healthcare system and education, and socioeconomic and health inequalities that progress CVD burden, in conjunction with Morocco’s progress in achieving its Sustainable Development Goals.
The Burden of Cardiovascular Disease (and NCDs) in Morocco
Cardiovascular Disease and Risk Factors Contribute to a Substantial Proportion of Mortality
The burden of cardiovascular diseases (CVDs) within Morocco constitutes a critical element of the country’s public health landscape. Several articles underscore this pressing concern shedding light on how cardiovascular diseases stand as a key driver behind a substantial proportion of NCD-related fatalities. The literature presents that ischaemic heart disease (IHD) was the top cause of death in the Arab world in 2010, which contributed to 14.3 percent of deaths.¹⁰ Through Mokdad’s method of dividing twenty-two Arab countries into low-income, middle-income, and high-income countries, they were able to estimate causes of death, disability-adjusted life years (DALYs), DALY-attributable risk factors, years of life lived with disability (YLDs), years of life lost due to premature mortality (YLLs), and life expectancy. Mokdad’s analysis of the burden of diseases, injuries, and risk factors in Morocco explains that since 1990, NCDs that directly impact cardiovascular health (ischemic heart disease (IHD), high blood pressure, obesity, etc.) have worsened.
Similarly, a comprehensive analysis of CVDs and associated risk factors in the Moroccan population reveals a staggering 38 percent mortality rate attributable to CVDs within Morocco.⁹ This analysis was conducted by a comprehensive literature review approach – delving into existing research and data, drawing insights from studies conducted in the Arab world, particularly within the context of Morocco’s evolving health landscape. IHD and stroke emerge as the primary risk factor – collectively responsible for over half of these fatalities.⁹ The prevalence of key risk factors within the studied population, notably tobacco smoking, physical inactivity, elevated hypertension rates, and even depression, signifies a complex interplay of lifestyle, socioeconomic factors, and health indicators contributing to this burden.⁹ Elyamani’s systematic review results align with Mokdad’s research reinforcing the substantial impact of cardiovascular diseases on Morocco’s public health landscape. The combination of broad-spectrum analysis, as seen in Mokdad’s study, and the precision and depth afforded by systematic review techniques in the second study, enriches the overall comprehension of the multifaceted aspects of CVDs and their implications for public health in Morocco. IHD maintains its significant presence authenticating Mokdad’s earlier findings that it is a leading cause of mortality in Morocco. Moreover, the identification of similar risk factors such as high blood pressure (although with varying prevalence rates) serves as a thread connecting the two studies.⁹-¹⁰ The systemic challenges mentioned in the epidemiological review such as high illiteracy rates, socioeconomic status, and inadequacies within the healthcare system concur with Mokdad’s analysis, hinting at potential catalysts fueling the exacerbation of CVDs and NCDs in Morocco over time.⁹
Results also suggest the concerning prevalence of risk factors among a cohort of young individuals, hinting at potential future implications for the broader cardiovascular health landscape in Morocco.³ The adoption of the STEPwise approach in Loukili’s study, endorsed by the WHO for monitoring NCD risk factors, highlights the commitment to standardized data collection, enabling strong comparability with similar global studies. Regarding the cardiovascular disease risk factors among young adults in Moroccan university setups, undiagnosed hypertension was prevalent (with a reported rate of 8.54 percent), diabetes (3.31 percent), and obesity (6.17 percent).³ The study’s identification of obesity as a significant concern mirrors the evolving trends in cardiovascular risk factors observed across various demographics in Morocco.
Conversely, the systematic review of Turkish and Moroccan migrant groups in Europe, employing a systematic search spanning 1950 to 2010 across peer-reviewed journals, highlighted a similar incidence of high obesity and diabetes rates among these populations compared to Western European demographics.⁷ The alignment of these findings from various demographic groups and geographical locations resulted in continuity in the prevalence of cardiovascular risk factors among Moroccan populations.⁷ This is irrespective of age or location. Both studies contribute findings on the prevalence and patterns of CVD risk factors. Loukili’s study among Moroccan young adults elucidates the early emergence of undiagnosed risk factors among a potentially influential and educated segment of the population, while Ujicic-Voortman’s systematic review highlights similar trends among migrant communities. This convergence of results underlines the importance of tailored interventions and proactive measures to address the observed risk factors within Moroccan populations. Both Loukili and Ujcic-Voortman assert that further research must delve into the underlying determinants and potential interventions to mitigate the burden of cardiovascular diseases among various demographic groups within Morocco and its migrant communities in Europe.
Across all studies, there is a resounding consensus that the Moroccan population confronts a significant array of cardiovascular risk factors that directly contribute to overall mortality rates and impact the quality of health. The convergence of findings from Mokdad’s comprehensive analysis, Elyamani’s literature review, Loukili’s examination of young adults in Morocco, and Ujcic-Voortman’s systematic review of migrant populations in Europe reveal a striking pattern. Ischemic heart disease consistently emerges as a leading cause of mortality (Figure 3).⁸ The shared risk factors such as high blood pressure, obesity, and diabetes intertwine these studies, showcasing the pervasiveness of these health challenges across different demographics and locations. The collective findings underscore a complex interplay of socioeconomic factors, lifestyle behaviors, and healthcare system nuances that contribute to the exacerbation of cardiovascular diseases and NCDs in Morocco.
The Challenges in Morocco’s Healthcare and Education System
Limited Access to Care and Disparities in Resource Allocation Contribute to Barriers
Editorials and publications address the limited access to quality medical care and disparities in resource allocation in Morocco (Figure 5).⁴-¹¹ These challenges are seen as barriers to managing and reducing the burden of cardiovascular NCDs.¹¹ Morocco’s escalating prevalence of NCDs further strains its healthcare system with factors like tobacco use, poor diets, and sedentary lifestyles significantly contributing to this burden, suggesting a need for comprehensive interventions to address lifestyle-related health risks.¹¹ An unequal distribution of healthcare resources, particularly between urban and rural areas, emerges as a prominent issue leading to disparities in access to healthcare infrastructure, medical equipment, and specialty care.¹¹ Mahdaoui’s findings display that financial constraints pose a substantial hurdle limiting essential medication access and impeding necessary improvements in healthcare infrastructure nationwide. The shortage of healthcare personnel, especially doctors and nurses, contributes to prolonged wait times for patients and limits access to specialized care in rural regions.¹¹
As previously mentioned, a study revealed that Moroccan immigrants in the Netherlands exhibited lower rates of hypertension, cardiovascular disease, and mortality.⁷ This contrast could potentially be associated with the differential accessibility and quality of healthcare systems between the Netherlands and Morocco. The discrepancy in healthcare access and system preparedness between these regions may contribute to varying levels of disease detection, management, and subsequent mortality rates among immigrant groups.⁷ This disparity draws a line regarding the influence of healthcare infrastructure and accessibility as contributing factors in determining cardiovascular health outcomes among different populations.
Mahdaoui and Ujcic-Voortman’s findings can be attributed to the health education model in Morocco. In Morocco, the predominant emphasis within the health education curriculum remained aligned with the biomedical model.¹² However, over the past decade, subtle inclusions from the social health model emerged, though these remained unnamed within the curriculum.¹² The slow integration of aspects from the social health model within health education signals a potential move toward a more comprehensive understanding of health beyond the traditional biomedical framework—potentially offering avenues for addressing the diverse challenges of Morocco’s healthcare system.¹²
Concurrently, Morocco’s participation in global efforts to combat NCDs through a national multisectoral strategy signifies proactive engagement.¹¹ However, NCDs constitute a staggering 80 percent of deaths in Morocco, with mortality rates among the highest in the region (Figure 4).⁴ It is necessary to reflect on the challenges listed with consideration in the educational model as one way to alleviate this predominant issue.
Socioeconomic and Health Inequalities and Progress Towards Sustainable Development Goals
Inequalities Exacerbating the Burden of Cardiovascular Diseases and Reaching SDG 3
The references mentioned highlight the presence of socioeconomic and health inequities in Morocco’s healthcare system exacerbating the burden of cardiovascular NCDs. However, many articles present findings that Morocco is slowly making progress toward achieving some of the SDG 3 targets.¹³ Examining how Morocco is implementing solutions may help with addressing the NCD burden (Figure 5).
Results from national surveys, government documentation, and information from UNICEF, WHO, United Nations Development Program, United Nations Population Fund, UNESCO, and the World Bank outline substantial strides in healthcare access and outcomes across the Moroccan population, particularly for mothers and children.⁶ Advancements in addressing health disparities and socioeconomic status were unevenly distributed across demographics and regions. ⁶ This publication highlights disparities between advantaged and disadvantaged areas, literate and illiterate women, rural and urban locales, as well as affluent and impoverished segments of the population.⁶ The main point from W. Boutayeb’s analysis is that socioeconomic and health inequalities are unfairly distributed between varying populations. These are the factors that exacerbate the burden of diseases like CVD and risk factors within Morocco.⁹
Regarding the costs associated with the management of NCDs in Morocco, a systematic search found that NCDs in countries that had higher healthcare costs for their government (Morocco), made it extremely difficult for families and individuals to afford quality healthcare.⁵ Although the findings had limitations in quantifying accurate costs, they demonstrate there is a substantial burden in accessing quality healthcare and preventing the progression of NCDs in Morocco.⁵-⁶ The diverse array of studies portrays a consistent narrative of persistent socioeconomic disparities in Morocco’s healthcare system. While advancements in healthcare access for certain mothers and children have been evident, these gains remain unevenly distributed across regions and population segments.¹³-⁶
This unequal distribution significantly exacerbates the burden of cardiovascular NCDs within Morocco.⁶ The strain of managing NCDs, coupled with high healthcare costs, impedes equitable access to quality healthcare.⁵ However, amidst these challenges, there has been research and investigation of gradual progress toward achieving Sustainable Development Goal targets. This offers a potential pathway to address the burden of NCDs by mitigating socioeconomic disparities in healthcare access and outcomes.
Morocco’s Progress in Reaching Goal 3: Good Health and Well-Being (UNICEF)
In a study that looked at SDG 3 health targets in six Arabic countries in North Africa, results indicated many challenges in achieving health targets across the Arabic North African countries.¹³ This is related to NCDs (which are reported to account for two-thirds of all deaths in low and middle-income countries), and suicide rates.¹³ While several nations faced challenges in achieving SDG 3 NCDs and suicide targets, Algeria and Morocco showed relative exceptions to these concerns.¹³ It is proposed that Morocco has done this by implementing radical changes such as the Riyadh Declaration in 2012. The progress toward SDG 3 emphasizes variations in health outcomes and highlights areas where specific countries, including Morocco, may demonstrate more promising trajectories in certain health indicators.¹³
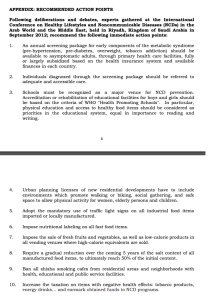
Based on the outcome of an international conference with the Ministry of Health of Saudi Arabia and the WHO Regional Office for the Eastern Mediterranean, there are results of the development and implementation of the UN Political Declaration on NCDs.¹⁴ In the Riyadh Declaration, there is an extensive focus on combating NCDs and listed recommendation action points (Figure 6). Some of these include more intensive primary care screening, health education in schools, increased nutritional information, and increased taxation on items with negative health effects.¹⁴ For Morocco, implementing these strategies stands pivotal in offering pathways for fortifying healthcare systems, fostering collaborations among diverse stakeholders, prioritizing public health interventions, and aligning national health agendas with global commitments like the Sustainable Development Goals. Embracing the Riyadh Declaration’s calls to action not only strengthens Morocco’s fight against NCDs but also aligns with broader global health objectives, propelling the nation toward achieving Sustainable Development Goal 3: Good Health and Well-Being.
Conclusions, Reflections, and Future Directions
Reflecting on the research question regarding the prevalence and impact of cardiovascular diseases in Morocco, the readiness and capacity of Morocco’s healthcare system, and potential interventions alongside health inequities, it is evident that cardiovascular diseases pose a substantial burden in Morocco. Studies by Mokdad and Elyamani highlighted the prevalence of ischemic heart disease and stroke, emphasizing the retrospective nature of the research methodologies. This calls for a more holistic approach blending qualitative and quantitative methods to capture real-time changes in lifestyle and socioeconomic factors impacting cardiovascular health. Moreover, exploring Morocco’s healthcare system readiness and capacity brought attention to disparities and limitations. Mahdaoui’s study underlined the barriers to access to quality medical care, emphasizing the unequal distribution of resources, while Ujcic-Voortman’s research shed light on healthcare disparities among Moroccan migrant groups. Despite progress, these studies highlighted the need for more nuanced analyses to capture contextual dynamics and ongoing interventions’ real-time impacts.
While the synthesis underscores the urgent need for tailored interventions and integrated healthcare strategies, it also highlights the importance of continued research to address the burden of cardiovascular diseases and healthcare disparities in Morocco. Adopting a multidimensional approach is critical to fostering a more equitable and resilient healthcare system, improving health outcomes, and reducing disparities among the Moroccan population.
References
- World Health Organization. Cardiovascular diseases. https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1.
- World Health Organization. Noncommunicable diseases. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases.
- Loukili H, et al. Cardiovascular Diseases Risk Factors Among Young Adults: A STEPwise-Approach-Based Study in Three University Setups in Morocco. Open Public Health J. 2020;13(1):464-469. doi:10.2174/1874944502013010464.
- Boutayeb A, ed. Disease Prevention and Health Promotion in Developing Countries. 1st ed. Springer International Publishing; 2020. doi:10.1007/978-3-030-34702-4.
- Saleh S, et al. Costs Associated with Management of Non-Communicable Diseases in the Arab Region: A Scoping Review. J Glob Health. 2018;8(2):020410. doi:10.7189/jogh.08.020410.
- Boutayeb W, et al. Actions on Social Determinants and Interventions in Primary Health to Improve Mother and Child Health and Health Equity in Morocco. Int J Equity Health. 2016;15:19. doi:10.1186/s12939-016-0309-9.
- Ujcic‐Voortman JK, et al. Obesity and Cardiovascular Disease Risk Among Turkish and Moroccan Migrant Groups in Europe: a Systematic Review. Obes Rev. 2012;13(1):2-16. doi:10.1111/j.1467-789X.2011.00932.x.
- Unicef. Unicef Data. Goal 3: Good Health and Well-Being. https://data.unicef.org/sdgs/goal-3-good-health-wellbeing/.
- Elyamani R, Soulaymani A, Hami H. Epidemiology of Cardiovascular Diseases in Morocco: A Systematic Review. Rev Diabet Stud. 2021;17(2):57-67. doi:10.1900/RDS.2021.17.57.
- Mokdad AH, et al. The State of Health in the Arab World, 1990–2010: An Analysis of the Burden of Diseases, Injuries, and Risk Factors. Lancet. 2014;383(9914):309-320. doi:10.1016/S0140-6736(13)62189-3.
- Mahdaoui M, Kissani N. Morocco’s Healthcare System: Achievements, Challenges, and Perspectives. Cureus. 2023;15(6):e41143. doi:10.7759/cureus.41143.
- Caussidier C, et al. In Search of a Health Education Model: Teachers’ Conceptions in Four Mediterranean Countries. Glob Health Promot. 2011;18(4):5-15. doi:10.1177/1757975911422962.
- Bjegovic-Mikanovic V, et al. A Gap Analysis of SDG 3 and MDG 4/5 Mortality Health Targets in the Six Arabic Countries of North Africa: Egypt, Libya, Tunisia, Algeria, Morocco, and Mauritania. Libyan Journal of Medicine. 2019;14(1):1607698. doi:10.1080/19932820.2019.1607698.
- World Health Organization – Eastern Mediterranean Region. International Conference on healthy lifestyles and noncommunicable diseases in the Arab world and the Middle East, Riyadh, 10–12 September 2012. https://www.emro.who.int/noncommunicable-diseases/ncd-infocus/riyadh-conference-september-2012.html.
- The Institute for Health Metrics and Evaluation. Morocco. https://www.healthdata.org/research-analysis/health-by-location/profiles/morocco
Appendix
Figure 1: Methods Process
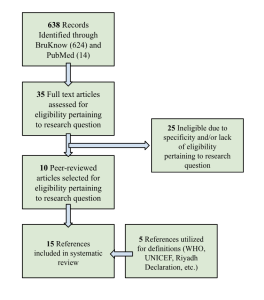
Figure 2: Overview of Sources
Figure 3: Morocco’s SDG Progress.¹⁵
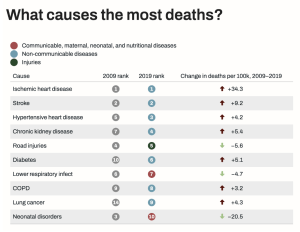
Figure 4: Causes of Death in Morocco from NCDs.⁴

Figure 5: Chronic Diseases and Risk Factors in Morocco.⁴
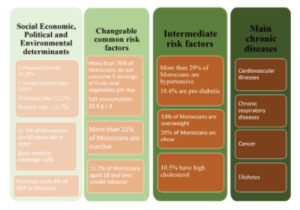
Figure 6: The Riyadh Declaration – 2012.¹⁴